Preventing sensitization by matching for HLA on the epitope level
HLA matching for clinical transplantation has remained unchanged for decades and is based on matching for HLA-A, -B and -DR on the antigen level. However, not HLA antigens but polymorphic amino acids (referred to as epitopes) present on mismatched HLA antigens are the targets for HLA antibodies. All HLA molecules harbor a set of epitopes, and while individual epitopes can be shared between HLA antigens, the total composition of epitopes is unique for a certain HLA antigen. Matching for epitopes rather than antigens can minimize the formation of donor specific antibodies (DSA), and thereby result in better long-term graft survival. However, before HLA epitope matching can be introduced in the clinical setting, it is pivotal to determine the relative immunogenicity of HLA epitope mismatches, since not all epitope mismatches are equally immunogenic. For HLA class I, our laboratory has generated over one hundred human monoclonal antibodies (mAbs) that have been used to verify the immunogenicity of individual HLA class I epitopes. We have recently developed a pipeline for the production of human recombinant HLA class II monoclonal antibodies (mAbs) with specificities covering HLA-DR, -DQ, and -DP. The reactivity patterns of these mAbs are extensively analysed to determine the reactive amino acids on HLA molecules with the aim to verify immunogenicity of individual epitopes. The generated mAbs are available for research purposes.
The second way of determining relative immunogenicity of amino acid polymorphisms on mismatched HLA is by analyzing large datasets of kidney transplant recipients who either did or did not form HLA antibodies upon transplantation. We have developed a computer program that can be used for analyzing donor and recipient HLA mismatches on the amino acid level, called HLA-EMMA (Epitope MisMatch Algorithm), which will be used to study the relative immunogenicity of epitope mismatches. This research is performed in the context of the 18th International HLA and Immunogenetics Workshop.
Detection of circulating HLA-specific memory B cells in transplant candidates
Sensitization against HLA can result in the formation of circulating HLA antibodies and/or the development of HLA-specific memory B cells. In recent years, work from our lab and others indicated that HLA antibodies can be present in the absence of (detectable) circulating memory B cells with accompanying specificity, or vice versa. In the latter situation, patients could erroneously be classified as not being sensitized to a prospective donor. To this end, we have developed several assays in our laboratory to determine the presence and specificity of HLA-specific memory B cells in the circulation. These assays are now used in the research setting to determine the clinical relevance of HLA-specific memory B cells in various clinical situations, such as repeat transplant candidates, husband to wife transplants, graft nephrectomies, and during desensitization therapies. One of the studies in which we currently are determing the clinical relevance of measuring HLA-specific memory B cells is the Dutch multicentre Procare 2.0 study, funded by the Dutch Kidney Foundation.
Transplanting highly sensitized patients based on acceptable HLA antigens
Highly sensitized patients have formed antibodies against the majority of HLA antigens present in the donor population, and are therefore extremely difficult to transplant. Within Eurotransplant, a special program for highly sensitized patients was initiated in 1989 in which highly sensitized patients are allocated kidneys based on proven acceptable antigens, instead of merely avoiding unacceptable antigens. The Eurotransplant Acceptable Mismatch (AM) program is coordinated by the Eurotransplant Reference Laboratory. We have recently shown that patients who received a kidney through this Acceptable Mismatch (AM) program have superior graft survival and a vastly reduced incidence of rejection episodes when compared with highly sensitized patients transplanted through regular allocation. Within the AM program, we are constantly analyzing outcome data to further improve allocation to highly sensitized patients. Furthermore, we are analyzing the epitopes present on acceptable HLA antigens to get a better understanding of which epitope mismatches may be non-immunogenic, and therefore acceptable.
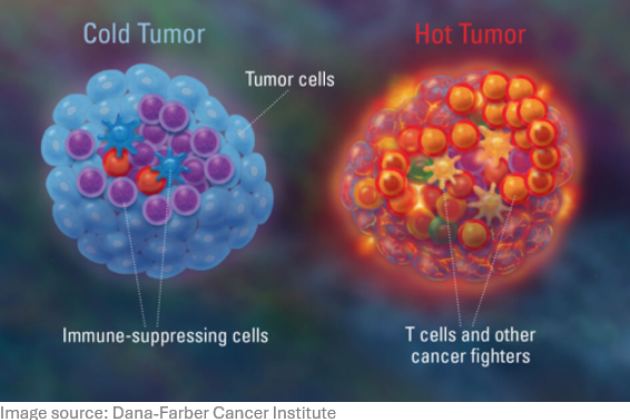
Novel treatment options for highly sensitized patients
Some highly sensitized patients are so difficult to transplant that even within special programs such as the Eurotransplant AM program they have minimal chance to receive a compatible donor organ. Currently, desensitization by using plasmapheresis in combination with B cell depletion is being used to create a window of opportunity to transplant. Since these therapies are non-specifically affecting the immune system of the patient and have varying degrees of success, novel and more specific treatment options are required. We are studying novel avenues of specifically targeting B cells with HLA specificity, without affecting B cells with other specificities.