Cancer-specific CD4 and CD8 T cell immunity
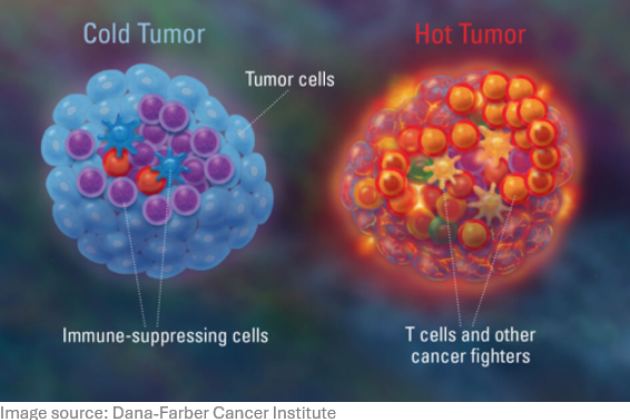
T lymphocytes are key in immune control of cancer, since they can specifically recognize and kill malignant tumor cells. Most current immunotherapies stimulate tumor-specific T lymphocytes in a non-specific way e.g., by immune checkpoint antibodies, now commonly used in the clinic. We aim to develop more specific immunotherapies with less side effects by identifying unique (neo)antigens in individual tumors, which are used to design patient-specific therapeutic vaccines. Using exome sequencing information and MHC peptide elution followed by mass spectrometry we can identify specific peptide sequences recognized by tumor-specific T cells.
Using these specific peptide epitopes we study the specificity and functionality of CD8 and CD4 T cells in the immune control of cancer using flow cytometry, high-end single cell assays and in vivo imaging methods. The central role of antigen-specific CD4 T cells and their immunomodulatory functions in the local tumor microenvironment and the tumor draining lymph nodes are subject of study.
Antigen presentation and dendritic cell biology
For optimal T cell activation, it is key to understand the processing and MHC presentation of antigenic peptides as well as the biology of dendritic cells in lymphoid and non-lymphoid tissues. We study antigen handling of dendritic cell subsets in relation to antigen processing pathways, subcellular trafficking and proteasome and peptidase activities. The effects of dendritic cell activation by innate signals like TLR signaling and interaction with CD4 T helper cells are studied. We aim to understand these processes to optimally activate T cell functions to eradicate cancer cells or modulate the tumor microenvironment for adequate immunotherapy.
Molecularly defined cancer vaccines
We use model antigens, oncogenic viruses and neoantigens to design molecularly-defined cancer vaccines. Vaccine delivery systems, such as Toll like receptor ligand-based dendritic cell targeting, liposomal nanoparticulate formulations and dissolvable microneedle arrays for intradermal administration are analyzed as cancer therapeutics in preclinical murine models. Cancer adjuvants and formulations are optimized for GMP-compliant procedures for clinical first-in-man applications. Recently, synthetic peptide-based T cell vaccines conjugated to chemically well-defined TLR ligands were in-house GMP prepared and used for immunotherapy of cancer patients.
Our aims are to combine powerful therapeutic vaccination, eliciting high numbers of tumor-specific effector T cells, with local amelioration of the tumor immune environment using immune checkpoint inhibition or with novel ablative treatments like photodynamic therapies, anticipated to result in major improvements of clinical benefit.
Our key collaborators within LUMC are the groups of R Arens, J. Borst, M. Verdoes (Immunology), T. van Hall, S. van der Burg, F. Speetjens, H. Gelderblom (Medical Oncology), N. de Miranda (Pathology), P. van Veelen (CPM), P. ten Dijke (CCB) and M. Jager (Ophthalmology), and R. Rissmann (CHDR). Within the University Leiden: D. Filippov, S. van Kasteren, J. Codee (Organic Chemistry) and J. Bouwstra (LACDR).