Field Studies
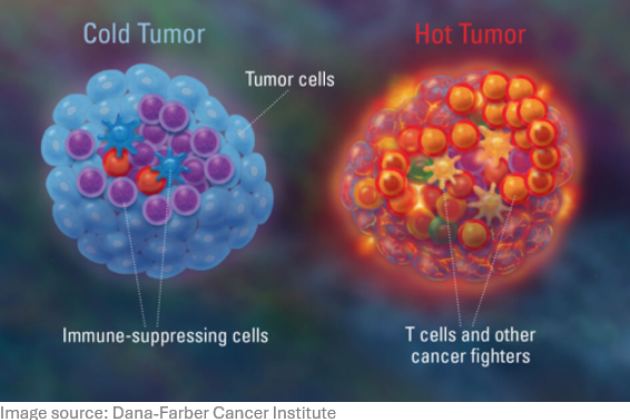
We investigate the impact of rural-to-urban lifestyle transitions on children's immune development and susceptibility to allergic and respiratory diseases. These transitions may lead to changes in environmental microbial exposure, air pollution, microbiome composition, and/or endemicity of gut helminth infections—once a natural component of the human microbiome. To study these effects, we conduct field studies in transitional areas such as Indonesia and Africa, in collaboration with local partners, including Hassanudin University (Makassar), Atma Jaya University (Jakarta), and Cermel (Lambaréné, Gabon). Our research focuses on allergic and respiratory symptoms, mucosal immunity, and systemic immune modulation in primary school children and adults.
References:
- Mbow M, et al. Immune responses to SARS-CoV-2 in sub-Saharan Africa and western Europe: a retrospective, population-based, cross-sectional study. Lancet Microbe. 2025 Feb;6(2):100942. doi: 10.1016/j.lanmic.2024.07.005. Epub 2024 Dec 18. PMID: 39708825.
- Chayé MAM, van Hengel ORJ, et al. Multi-dimensional analysis of B cells reveals the expansion of memory and regulatory B-cell clusters in humans living in rural tropical areas. Clin Exp Immunol. 2025 Jan 21;219(1):uxae074. doi: 10.1093/cei/uxae074. PMID: 39129562.
- Schmiedel Y, et al. CD4+CD25hiFOXP3+ Regulatory T Cells and Cytokine Responses in Human Schistosomiasis before and after Treatment with Praziquantel. PLoS Negl Trop Dis. 2015; 9(8):e0003995. doi: 10.1371/journal.pntd.0003995. PMID: 26291831.
Clinical Studies
Epidemiological research has demonstrated significant geographical differences in the incidence of allergies and childhood asthma. Factors such as growing up on small family-run farms, proximity to green spaces, and diets rich in complex fibers with minimal refined carbohydrates are associated with a reduced risk of inflammatory diseases. We engage in clinical (intervention) studies to move beyond correlation and establish causality.
Through clinical collaborations, we investigate dietary interventions (e.g., the MARTHA trial on farm milk), and microbial exposure interventions (e.g., the Protea study on bacterial lysates) as well as the immune impact of controlled allergen (house dust mite) or viral infections (rhinovirus). These studies examine immune development systemically and at the nasal mucosa in relation to microbiome composition and respiratory health outcomes. Additionally, we perform in-depth single-cell analyses of nasal mucosal immunity in cohorts of people with allergic rhinitis, asthma, COPD, and COVID-19 to identify immune deviations associated with respiratory disease severity. Our research employs advanced methodologies such as mass and spectral flow cytometry, transcriptomics, and secretomics.
References:
- van Duuren IC, van Hengel ORJ, et al. The developing immune system in preterm born infants: From contributor to potential solution for respiratory tract infections and wheezing. Allergy. 2024 Nov;79(11):2924-2942. doi: 10.1111/all.16342. PMID: 39382056.
- Voskamp AL, et al. Inflammatory and tolerogenic myeloid cells determine outcome following human allergen challenge. J Exp Med. 2023 Sep 4;220(9):e20221111. doi: 10.1084/jem.20221111. PMID: 37428185.
- Roukens AHE, et al.Prolonged activation of nasal immune cell populations and development of tissue-resident SARS-CoV-2-specific CD8+ T cell responses following COVID-19. Nat Immunol. 2022 Jan;23(1):23-32. doi: 10.1038/s41590-021-01095-w. PMID: 34937933.
- von Mutius E, Smits HH. Primary prevention of asthma: from risk and protective factors to targeted strategies for prevention. Lancet. 2020 Sep 19;396(10254):854-866. doi: 10.1016/S0140-6736(20)31861-4. PMID: 32910907.
Preclinical Models
We employ sophisticated in vitro and in vivo models to dissect the complex molecular mechanisms underlying immune modulation by environmental and gut-derived microbes. Using primary human cells and animal models of allergic airway inflammation, we investigate how helminth infections, helminth-derived molecules, airborne microbes, farm dust, and gut microbial metabolites influence immune responses.
Our studies focus on dendritic cells, macrophages, and primary bronchial and nasal epithelial cells, employing co-culture models to explore immune interactions in allergic inflammation, asthma, and rhinovirus infections. These approaches provide mechanistic insights into local immune regulation at mucosal surfaces, contributing to the development of novel targeted therapeutic strategies.
References:
- Patente TA*, Gasan TA*, et al. S. mansoni -derived omega-1 prevents OVA-specific allergic airway inflammation via hampering of cDC2 migration. PLoS Pathog. 2024 ;20(8):e1012457. doi: 10.1371/journal.ppat.1012457. PMID: 39186814.
- Schrumpf JA, et al. Farm Dust Exposure Reduces Cytokine- and Rhinovirus-Induced IL-33 Expression in Bronchial Epithelial Cells. Clin Exp Allergy. 2024 Oct;54(10):766-769. doi: 10.1111/cea.14535. PMID: 38955345.
- Kuipers ME, et al. DC-SIGN mediated internalization of glycosylated extracellular vesicles from Schistosoma mansoni increases activation of monocyte-derived dendritic cells. J Extracell Vesicles. 2020;9(1):1753420. PMCID: PMC7241508.
- Haeberlein S, et al. Schistosome egg antigens, including the glycoprotein IPSE/alpha-1, trigger the development of regulatory B cells. PLoS Pathog. 2017 Jul;13(7):e1006539. PMCID: PMC5550006.
Partners / Collaborators
- Prof Markus Ege, Technical University Munich, Germany, involving clinical studies with minimally processed milk in children.
- Prof Pieter Hiemstra and Dr. Anne van der Does, PulmoScience Lab, LUMC, involving mucosal models with human primary bronchial and nasal epithelial cells and respiratory viral infections.
- Prof Ron Hokke, LUCID, involving molecular characteristics of helminth parasites.
- Dr. Simon Jochems, LUCID, LUMC, involving respiratory viral infections and systems tissue immunology.
- Prof Gerard Koppelman and Prof Martijn Nawijn, UMCG, Groningen, on how environmental threats influence the function of respiratory epithelium in infants suffering from pre-asthma.
- Prof Andrew MacDonald, University of Edinburgh, UK, on mucosal immunity in the lung and gut by schistosome helminths.
- Prof Rick Maizels and Dr Henry McSorley, University of Glasgow and Dundee, UK, on immunomodulation by helminth parasites and their molecules.
- Prof Ben Marsland, Monash University, Australia, involving the role of gut metabolites in the gut-lung axis.
- Prof Erika von Mutius, Helmholz Institute, Munich, Germany, on the immunomodulatory role of farm dust in the airways.
- Dr. Arjen Speksnijder, Hogeschool Leiden, involving airborne biodiversity and the impact on the immune system.
- Dr. Gerdien Tramper, Franciscus Gasthuis, Rotterdam, involving the use of bacterial lysates in protection against respiratory infections in moderate-late preterm infants.
- Ingrid de Visser, CHDR, Leiden, regards clinical studies involving metabolites and controlled rhinovirus infections.
- Prof Maria Yazdanbakhsh, LUCID, LUMC, together with Dr. Maria Kaisar and Prof Sitti Wahyuni, Atma Jaya, Jakarta, Indonesia, and Hassanudin Universitas, Makkasar, Indonesia, respectively, and Prof Akim Adegnika, Cermel, Gabon, involving human studies in rural and urban areas in Indonesia and Africa.